Rizia Bardhan, associate professor of chemical and biological engineering, recently received three awards totaling $2.25 million to support her innovative research program in engineered medicine. Bardhan has secured National Institute of Health (NIH) R01 and R21 awards, and an Idea award from the Department of Defense Congressionally Directed Medical Research Program (CDMRP) to advance her core research expertise in integrating nanoparticles and Raman spectroscopy to improve disease diagnostics and treatment.
“Since joining Iowa State just months ago, Rizia has already made her mark as a forward-thinking researcher whose engineering discoveries are will make a positive, lasting impact on human health, said Andrew Hillier, Reginald R. Baxter Endowed Department Chair in Chemical and Biological Engineering. “These awards to support Rizia’s efforts demonstrate just how creative and impactful her research program is – and how Iowa State engineering students have the opportunity to learn from and get hands-on research experience with the very best faculty.”
Predicting immunotherapy success

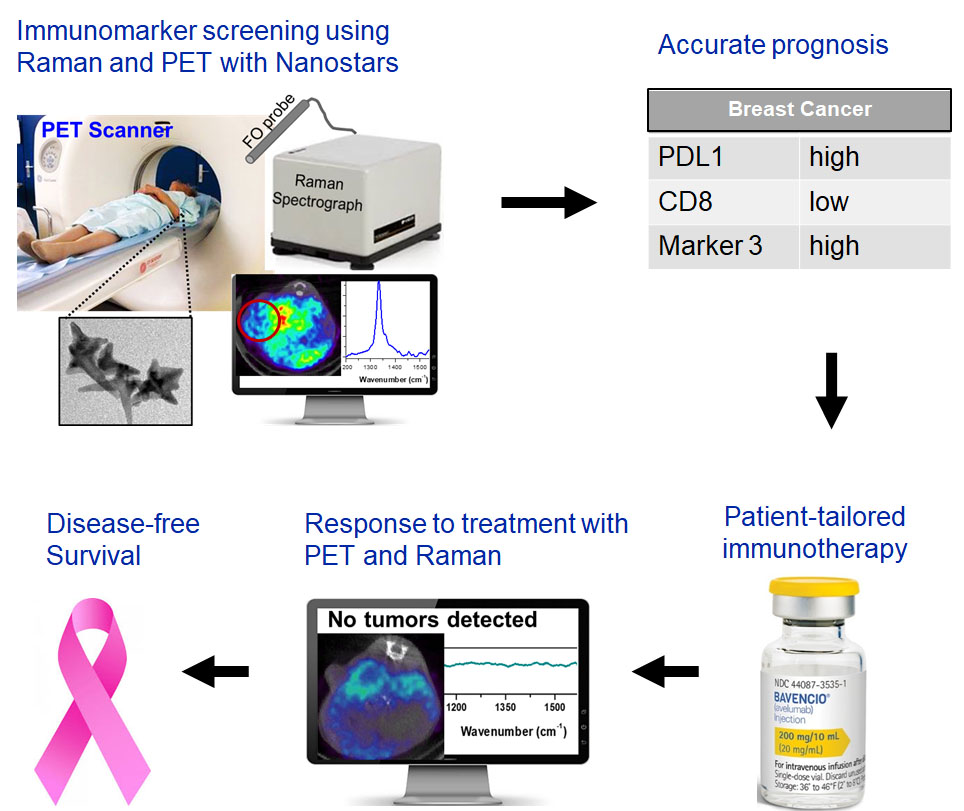
In one of the NIH awards, Bardhan will transform the way immunotherapies are performed in cancer patients. Immunotherapy is a ground-breaking, Nobel Prize-winning new treatment for cancer and other immune system related diseases; however, right now only 20-25 percent of patients respond to immunotherapies. And no current diagnostic approach exists to help predict who will respond to treatment or to evaluate effectiveness during treatment, mostly because current clinical standard biopsy histopathology is not able to account for the immune biomarker PD-L1.
Bardhan will use an image-guided approach to solve this challenge by designing immunoactive gold nanostars, tiny particles that are about 500 times smaller than a strand of human hair. The gold nanostars will combine two medical imaging techniques, Positron Emission Tomography (PET) and Raman spectroscopy, that are widely used in guiding clinical therapies.
These nanostars will simultaneously detect both tumor cells expressing PD-L1 biomarker and also immune cytotoxic CD8 T cells directly in real time in vivo in animal models engrafted with breast cancer patient tumors.
“By tracking both cell types, our approach will help oncologists determine which patients are good candidates for immunotherapies and distinguish those who will not respond even before the start of treatment,” said Bardhan.
Bardhan will collaborate on this project with Dr. Anna Vilgelm at Ohio State Medical School and Thad Wadas at the University of Iowa. Bardhan recently published a paper in ACS Nano demonstrating these immunoactive nanoparticles.
Tailored colorectal cancer treatment
Leveraging the strengths of Raman spectroscopy as a cancer diagnostic, Bardhan’s DOD CDMRP Idea award will study how colorectal cancer (CRC) patients will respond to molecular therapies before treatment is administered in patients.
Metastatic CRC is highly lethal with limited treatment options and a 5-year survival of only about 11 percent. Early, accurate, and rapid diagnostic tools that can guide treatment choices are therefore necessary to ensure patients receive the most effective treatment at the earliest time point.
Bardhan is collaborating with Jonathan Mochel, associate professor of biomedical sciences at Iowa State’s College of Veterinary Medicine; Soumik Sarkar, Iowa State associate professor of mechanical engineering; and Bhuminder Singh at Vanderbilt University School of Medicine.
But how will they determine which is the best treatment for each patient? Bardhan’s answer is using “organoids,” which are 3D culture systems that closely capture the human tumor microenvironment and have revolutionized the drug development pipeline in multiple diseases.
“Drug discovery studies often use the ‘one mouse, one patient’ paradigm, where each mouse is engrafted with an individual patient tumor as an avatar for human tumor response. But such an approach is ineffective for timely clinical decisions because they are expensive, time-consuming, and inherently low-throughput,” said Bardhan.
Bardhan and her team will derive more than 100 organoids from each patient tumor and treat them with a panel of drugs, some of which are both standard of care in CRC patients and others in clinical trials. They will then perform high-throughput drug screening in these organoids with Raman spectroscopy, and apply machine learning to distinguish patients that will respond to drugs from the nonresponders.
Their approach will not only enable individualized treatment planning for each CRC patient, it will also decrease animal burden and read-out times, which are current challenges in drug efficacy studies. Bardhan’s team recently published a paper in Chemical Science demonstrating Raman spectroscopy-based screening in cancer cells.
Early, accurate, affordable preterm labor screening
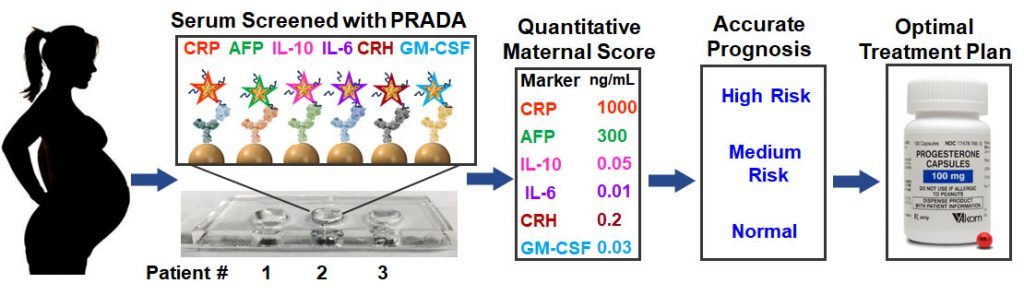
Bardhan’s expertise in Raman spectroscopy and nanoparticles also extends far beyond cancer. Her NIH R21 award is focused on the development of a cutting-edge new technology in her lab, PRADA, or portable reusable accurate diagnoses with nanostar antennas, to detect biomarkers that lead to spontaneous preterm labor in pregnant patients.
Preterm labor occurring before 37 weeks gestation results in more than 1 million childhood deaths globally under the age of 5. The current clinical standard to identify women at high risk of preterm labor has not been successful in reducing neonatal deaths. Bardhan’s approach with PRADA will address this ongoing global clinical challenge.
The PRADA diagnostic platform consists of the same gold nanostars Bardhan’s team uses in other research efforts, but they are now labeled with targeting agents, such as peptides or antibodies, and Raman molecules to allow multiplexed detection of clinically relevant biomarkers with high sensitivity and specificity. PRADA is also reusable, allowing more than 15 uses of the same sensor chip, reducing the overall cost.
Bardhan has also teamed up with Dr. Mark Santillan at the University of Iowa Carver College of Medicine Department of Obstetrics and Gynecology and Dr. Jeff Reese at Vanderbilt University School of Medicine to generate a unique “PRADA maternal risk score” by studying patient serum both at risk of preterm labor and those with normal pregnancy.
PRADA can ultimately enable early, accurate and affordable bedside screening for pregnant patients, which is a game-changer compared to current clinical measures. Bardhan’s team recently published a paper on this work in Bioengineering and Translational Medicine demonstrating PRADA in patient samples.