
For Iowa State chemical and biological engineering professor Derrick Rollins, a diagnosis of type II diabetes was a life-changing experience – but in one way you might not expect. In addition to the customary lifestyle changes that go along with such a diagnosis, Rollins has used his personal situation to launch a major research project that he hopes will one day allow diabetes patients to better understand the “hows” and “whys” of their blood glucose levels.
“When I was diagnosed with diabetes, I was given a glucose meter, and lots of lessons in what to eat, how to eat, and how to use the meter. But it was all just sort of blanket advice, the same advice they give everyone. They say to do this, cut down on that, but I saw inconsistencies with my glucose levels and sometimes didn’t know why, and thought ‘there has to be a better way of doing this where you are treated as an individual.’”
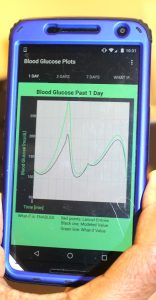
And so Rollins began the pursuit of an idea that would incorporate Bluetooth and smart phone technology to help individuals with Type II non-insulin dependent diabetes to not only simply track their blood glucose levels, but to develop a better understanding of how different things influence it. “I want to be able to introduce the ‘what if’ factor to checking your glucose,” he said. “’What if I ate that big cookie?’ ‘What if I work out at the gym today?’ ‘What if I do this thing instead of that thing, how will it affect my blood glucose?’” These factors would wind up as a sort of graph displayed on the patient’s smart phone through an app. “We know that eating a big meal will make your blood glucose rise,” Rollins said, “But with this idea you will able to get a line on a chart – a graphic estimate of how much it will rise that you can hold in your hand and understand.” This information will be displayed continuously for the user – not just what is revealed in the moment after a finger stick and blood collection. “Is there a certain time of day when you are stressed? This can confirm that and what it does to your glucose levels. Did you just walk three miles instead of one? This can show what that does for your glucose levels.”
Rollins, who is also a professor of statistics at Iowa State, would base his program on a mathematical model, which would be custom tailored for different people. Rollins collected data from his own blood as a starting point for developing a baseline which could be used to develop the plan. “The whole idea is, it takes information and allows us to infer what blood glucose will be as a result of an action, because it is based on a mathematical model.”
The idea to display inferences and changes in a person’s glucose on a cell phone came about out of a need to better illustrate just what his final vision would look like, Rollins related. “People just could not grasp the concept of what I wanted to do by just presenting it on paper,” he remarked. “The phone serves as a demonstration device. I need to have something that people can hold in their hands and be able to say, ‘OK, I see how this works.’”
The ability for people to see how the idea would work is important, as Rollins will need to secure funding to develop it – and to work with diabetics who must obtain and analyze their blood four times per day – with the difference being their blood analysis would be transmitted to the cell phone app. This is where the Bluetooth technology comes in. Through a hand-held Bluetooth transmitter, the patient will insert the test strip with a blood sample in one end of the device, and it will then send an analysis to the phone app, where it can be displayed on the phone screen. All automatically. “We are wanting to make this as automated as possible to reduce human error,” said Rollins.

All this cyber ability had to be created. And with the help of undergraduate students – both current ISU CBE students and those participating in special research opportunities – and graduate students, that is happening. “I had a couple of freshman honor students I worked with who I instructed to write the app for the Bluetooth device to connect with the phone. And they got that job done,” said Rollins proudly. Current development work finds three students from Des Moines Area Community College with the Research Innovation in Science Enrichment University Program (RISE UP) teaming to build the interface for the glucose pages in the phone app. They are continuing the work an undergrad research student in ISU’s Biological Materials and Processes Research Experience for Undergraduates (BioMaP REU) program did in developing all the pages for the interface. This summer, students are writing code for everything to be able to go into a phone.
The big future step for the project would be securing the means to do a study on a large group of subjects – probably 150-200 people, according to Rollins. Data would be collected from those individuals over a four-week period and downloaded in order to build a library that can then be used to establish parameters to use for the math-based inferences. “This would require a large grant, the type that researchers sometimes get from the National Institute of Health,” said Rollins.
Rollins regularly visits Ukraine, and there he sees many people who suffer from diabetes because of a lack of proper health care, improper diet, and a lack of proper education about diabetes and the effect different foods and drinks have on the disease. “My vision is to be able to go into places like Ukraine, or wherever people need help, and to develop the kind of relationships needed with health care officials to be able to give away materials and educate people on how to use the app and software I’m developing.”
“I want this technology to be available to people cheaply, so they can better know their glucose levels and make real-time decisions. It will be like having a virtual, online doctor, allowing them access to real-time data that is subject-specific, not blanket advice.
“This is a whole new concept. It’s chemical engineering modeling. It’s highly sophisticated research and no one has seen anything quite like this. We need to get people to accept it, and that’s why it’s important to get a device I can put in people’s hands to show them. If I give this to a diabetic person they are going to get excited about it, because they will realize it is something that will help them.”