Last fall, Iowa State University Palmer Department Chair in Electrical and Computer Engineering and Anson Marston Distinguished Professor David C. Jiles announced a groundbreaking research and development partnership between Iowa State University and the Steptoe Group, LLC. The partnership focuses on bioengineering of new diagnostic and treatment interventions in several brain disorders. The joint R&D efforts will initially target Deep Brain Transcranial Magnetic Stimulation (TMS) and Transcranial Ultrasound Stimulation in Traumatic Brain Injury, Post Traumatic Stress Disorder (PTSD), and Depression.
As of 2008, more than two million soldiers had served in Iraq and Afghanistan. Of those two million soldiers, more than 320,000 have some degree of Traumatic Brain Injury and over 300,000 have PTSD.
“Traumatic brain injury can occur when improvised explosive devices (IEDs), or roadside bombs, go off. The IEDs radiate shock waves that can travel through the brain, causing skull movement and the loss of brain function,” Steptoe says. “Traumatic brain injury can speed up the development of diseases, such as PTSD, depression, Parkinson’s Disease, vascular dementia, stroke, and more.”
The Steptoe Group, LLC, based in Ellicott City, Maryland, was founded in 2008 as a Service Disabled Veteran Owned Business whose objective is to create sustainable partnerships with government agencies and private organizations in order to improve access and delivery of quality health, science, and education services to military veteran and servicemen families.
According to Ron Steptoe, CEO of the Steptoe Group, their research focuses on individualized patient care. “Our major issue is that what works for some people doesn’t work for everyone. We are looking to find new ways, and developing a training program, to look at patients based on characteristics such as their age, gender, ethnicity, work, environment, and more.”
Currently, the company is working to increase awareness of the growing and detrimental impact mental health and behavioral mental health conditions are having on the military and veteran communities, as well as deliver unique technologies to improve injury recuperation.
“What we’re doing is developing transcranial magnetic stimulation (TMS) for deep brain stimulation—a non-invasive, non-surgical method for examining and treating the brain with minimal associated risk,” Jiles explains. “It is very promising because it enables you to treat someone’s brain without doing any surgery. It is not going to solve every problem that is out there, but our objective is to find out what it works for and to improve technology to treat brain disorders.”
Jiles’ research on TMS began about three years ago at Cardiff University. “I was interested in finding out how magnetics could be used in the biomedical field, and an opportunity came up when Magstim, a company that provides instrumentation, got a TMS device and needed some help to improve it,” Jiles says. “The device was relatively new and wasn’t doing quite what they wanted, so Magstim came to me and set up a research program to look at things like coil development, my area of expertise.”
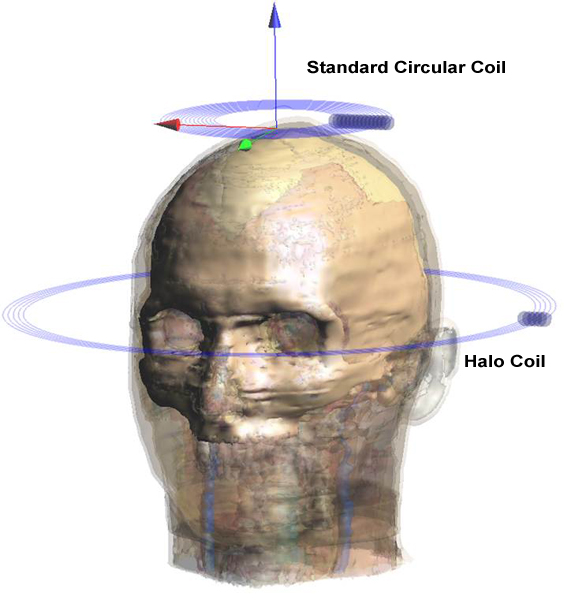
According to Jiles, the coils, which are put on the patient’s head to stimulate the outer part of the brain, were working, but overstimulated the surface when they tried to get deep brain stimulation. This was not only painful, but caused more effects on the outer part of the brain than they wanted and did little to stimulate the inside.
After two years, Jiles and team members Lawrence Crowther, graduate student in electrical engineering; Ravi Hadimani, postdoctoral research associate; and Paul Williams of Cardiff University, came up with a coil design and published their findings. While they found that the field penetrated very differently than they initially expected, they were able to rework their coil designs to reach inside the brain, increasing the field strength by a factor of four at 70 mm.
When the coils were tested on a number of patients suffering from several different brain disorders, the results showed some interesting effects. “By stimulating the brain, you can cause involuntary movement in the limbs, which is beneficial for stroke rehabilitation,” Jiles explains. “When paralysis occurs, muscle tone deteriorates. You can stimulate muscles using TMS to recover some of the muscle toning.”
In an ischemic stroke, the blood supply to the brain is cut off. If the individual survives, the blood supply is restored but the victim will suffer from brain damage. “TMS can be used to treat this because it ‘bathes’ the entire brain in a magnetic field, which stimulates the entire brain and not just the outer region,” Jiles says.
Preliminary results also suggest that TMS could be used as an alternative or even a possible replacement for electroconvulsive therapy (ECT), a method for treating severe depression. Tests done in hospitals showed that TMS worked just as well as ECT, but seemed to cause fewer side effects, which can include confusion and memory loss.
In addition, they found that stimulating certain parts of the brain can cause interruptions in individuals’ speech, while stimulation of other regions significantly improves individuals’ ability to perform simple mathematics on a temporary basis.
Kanthasamy, an expert on animal diseases—specifically Parkinson’s Disease and other neurodegenerative diseases — will aid in the research by testing the efficacy of the non-invasive magnetic field in an animal model of Parkinson’s Disease, while Bigelow will investigate transcranial ultrasound stimulation in the treatment of traumatic brain injury.Other Iowa State faculty members working on the project include Anumantha Kanthasamy, a distinguished professor of biomedical sciences and the W. Eugene and Linda R. Lloyd Endowed Chair in Neurotoxicology at the Iowa State University College of Veterinary Medicine, and Timothy Bigelow, assistant professor in electrical and computer engineering.“We will determine the ultrasound thresholds for brain stimulation both with and without an accompanying electromagnetic field,” Bigelow says. “While considerable work has been done showing that it is possible to stimulate neurons with ultrasound, the thresholds have not been explored when a magnetic field was also applied. Therefore, we will systematically explore the ultrasound parameters necessary for brain stimulation in both in vitro and in vivomodels both with and without a magnetic field.”Jiles adds that the potential benefits of the research and development partnership with the Steptoe Group are enormous. “Let’s find out what we can do non-invasively, optimize that, and bring it to its best capabilities,” Jiles says.While the partnership is still in its early stages, the team members are already hard at work pursuing funding sources, including the U.S. Department of Defense, National Institutes of Health (NIH), National Science Foundation (NSF), and Roy J. Carver Charitable Trust, among others.